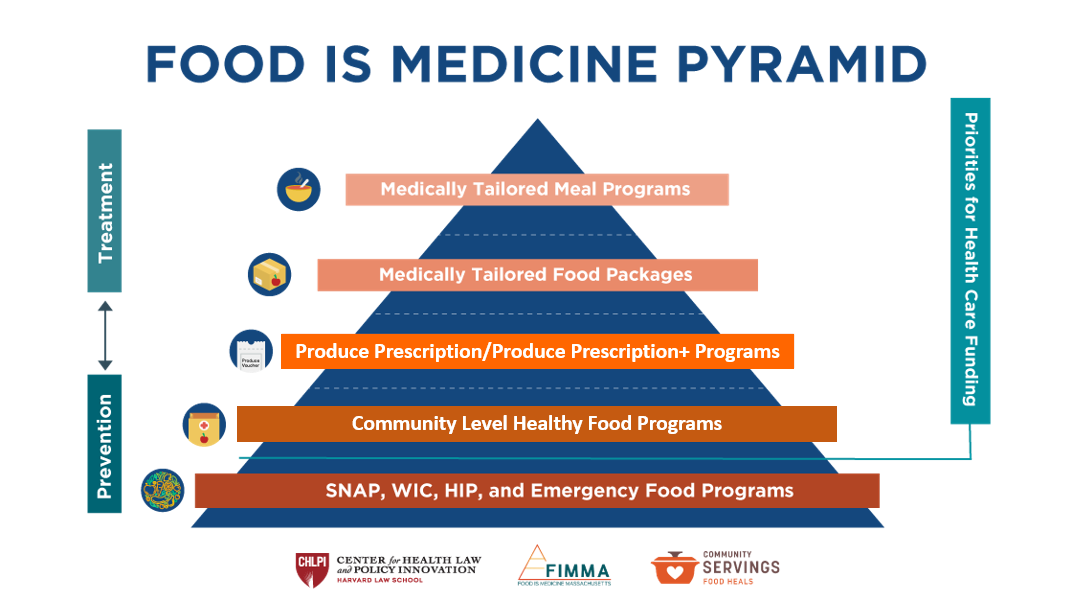
Lack of reliable access to sufficient, nutritious food is a key driver to health outcomes and related costs for Massachusetts residents. Food is Medicine refers to a spectrum of services and health interventions that recognize and respond to the critical link between nutrition and chronic illness.
Although Food is Medicine interventions often target food insecure populations, they are distinct from broader hunger safety net because of their focus on nutrition for chronic disease prevention, management, and treatment. A growing number of health care payers (i.e., public and private health insurers), providers (i.e., physicians, nurses, dietitians), and health systems (i.e., hospitals, community health centers) are now exploring how they can integrate Food is Medicine interventions into patient-centered models of care for individuals living with or at risk for complex chronic illnesses.
Improving access to nutrition safety net programs such as the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) can help combat food insecurity. However, for individuals coping with or at risk for chronic health conditions, these programs may not go far enough in preventing or treating illness.
By addressing nutritional needs within the context of health care, Food is Medicine interventions play an important role in preventing and/or managing many of the chronic conditions that drive health care costs across the Commonwealth, including: diabetes, cardiovascular disease, kidney disease, certain cancers, HIV, and more.
FIMMA Food is Medicine Definitions
Medically Tailored Meals
Medically tailored meals (MTM) are meals developed to address the dietary needs of an individual’s medical condition by a Registered Dietitian Nutritionist. Individuals are referred by a healthcare provider or plan.
Medically Tailored Food Packages
Medically tailored food packages (MTFP) include a selection of minimally prepared grocery items selected by a Registered Dietitian Nutritionist or other qualified nutrition professional as part of a treatment plan for an individual with a defined medical diagnosis. The recipient of a medically tailored food package is typically capable of shopping for and picking up the food and preparing it at home, and is referred by a healthcare provider or plan.
Produce Prescriptions/Produce Prescriptions+
Produce prescriptions/produce prescriptions+ (PRx/PRx+) provide funds for free or discounted nutritious foods. Individuals must receive referrals from healthcare providers or plans after being identified as having or being at risk for diet-related diseases.
Community-Level Healthy Food Programs
Community-level healthy food programs (CLHFP) provide nutritious foods for a population that currently has or is at increased risk for chronic disease associated with food insecurity. These programs are done in partnership or consultation with a healthcare payer, provider or nutrition professional, for screening or referrals, and/or in program design, management, or evaluation.
FIMMA Definitions and Standards Project
Data collection for the State Plan report showed that the lack of consensus on nutrition standards, quality, and client/patient eligibility for various services is a barrier to scaling success to Food is Medicine interventions. Without consistent definitions and standards, it is difficult for providers to understand which services are most appropriate for patients with different health profiles. The Community Based Organization (CBO) Task Force leads a statewide effort to establish standards for Food is Medicine interventions in the Commonwealth (Recommendation #7 of The Massachusetts Food is Medicine State Plan).
Goals
These definitions and standards will provide guidance to CBOs, health care payers, health care providers, and consumers for the purpose of:
- Expanding access to Food is Medicine interventions to individuals at risk for or coping with diet-related chronic illness;
- Investing in and scaling Food is Medicine interventions;
- Expanding health insurance reimbursement of Food is Medicine interventions;
- Referring consumers in the health care setting to the appropriate nutrition resource in the community.
Contact us to learn more about this project.
National Food is Medicine Initiatives
Food is Medicine Coalition
The Food is Medicine Coalition (FIMC) is a coalition of nonprofit, medically tailored food and nutrition services providers from across the country. The goal of FIMC is to advocate for public policy that supports access to food and nutrition services for people with critical and chronic illnesses. Learn more about FIMC and how to get involved.
National Produce Prescription Collaborative
With support from Wholesome Wave, the National Produce Prescription Collaborative (NPPC) launched in 2019 to support and leverage Produce Prescription programs as prevention & intervention for diet-related disease through federal policy change and further embedding this effective model into healthcare and community food systems.
Aspen Institute’s Food & Society Food is Medicine Initiative
The Aspen Institute’s Food is Medicine Initiative aims to expand access to proven interventions. The Initiative brings together key players from across the country to share existing knowledge and expertise, identify critical gaps and strategic priorities, and facilitate new collaborations in underrepresented regions and communities. Food and Society, working in close collaboration with its expert Food is Medicine Advisory Board, published the Food is Medicine Research Action Plan.
GusNIP Nutrition Incentives Hub
The Nutrition Incentive Hub was created by the GusNIP NTAE Center to provide training, technical assistance, reporting, and evaluation support to GusNIP grantees toward the intended impact of increasing the purchase of fruits and vegetables by produce prescription programs and nutrition incentives.